Do you snore loudly, feel tired during the day, or wake up gasping for air? If so, you might have sleep apnea, a common but serious condition that affects your breathing while you sleep. Sleep apnea can increase your risk of heart disease, stroke, diabetes, and other health problems.
The good news is that sleep apnea can be diagnosed and treated. One of the ways to find out if you have sleep apnea is to do a sleep apnea test at home. This is a convenient and affordable option that allows you to monitor your sleep in the comfort of your own bed.
In this article, we will explain everything you need to know about home sleep studies, including what they are, how they work, what they measure, how to prepare for them, and more.
What is an at home sleep test?
An at home sleep test (also called a home sleep apnea test or HSAT) is a device that you use to record your sleep patterns and breathing at night. It is a simplified version of polysomnography (PSG), which is the gold standard test for diagnosing sleep apnea in a sleep lab.
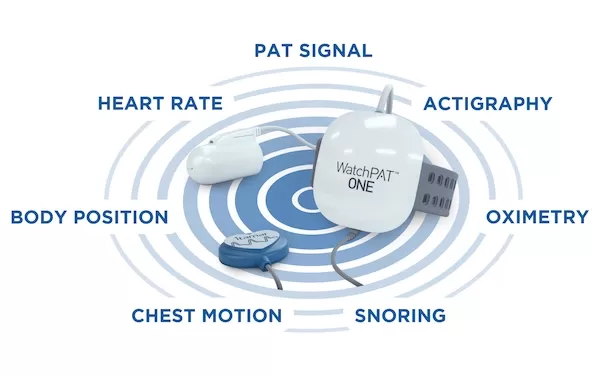
An at home sleep test usually consists of a small device that you wear on your chest or wrist, a nasal cannula (a tube that goes under your nose), and sometimes a finger pulse oximeter (a clip that measures your blood oxygen level). Some of the latest at home sleep test devices, like those sold by Lofta, are simple watches or rings that gather your sleep data and send them to your healthcare provider via an app.
The device collects data such as your airflow, breathing effort, snoring, heart rate, oxygen saturation, and body position. It does not measure your brain waves, eye movements, or muscle activity like a PSG does. Therefore, it cannot detect other types of sleep disorders such as insomnia, narcolepsy, or restless legs syndrome.
An at home sleep study is designed to diagnose obstructive sleep apnea (OSA), which is the most common form of sleep apnea. OSA occurs when your throat muscles relax and block your airway during sleep, causing you to stop breathing for short periods of time. This can happen hundreds of times per night and disrupt your sleep quality and oxygen levels.
How does a sleep test at home work?
An at-home sleep test is easy to use and does not require any special training or supervision. You can get one from your doctor, a sleep specialist, or an online provider. Here are the basic steps involved in doing an at home sleep test:
Before the test, you will receive instructions on how to set up and use the device. You may also have to fill out some questionnaires about your medical history, symptoms, and medications.
On the night of the test, you will follow your normal bedtime routine and attach the device as instructed. You will turn on the device before going to sleep and leave it on until you wake up in the morning.
In the morning, you will turn off the device and remove it. You will return the device to the provider or mail it back using a prepaid envelope. The provider will download the data from the device and analyze it using software or send it to a board-certified sleep physician for interpretation.
Within a few days, you will receive a report with your results and recommendations. The report will include metrics such as your apnea-hypopnea index (AHI), which is the number of times per hour that you stop breathing or have shallow breathing; your oxygen desaturation index (ODI), which is the number of times per hour that your blood oxygen level drops below a certain threshold; and your respiratory disturbance index (RDI), which is the number of times per hour that you have any type of breathing disruption. The report will also indicate if you have mild, moderate, or severe OSA based on these metrics.
Based on the results of your at home sleep test, you may be advised to start treatment for OSA such as continuous positive airway pressure (CPAP) therapy, oral appliances, surgery, or lifestyle changes. You may also be referred to a sleep specialist for further evaluation or confirmation of your diagnosis.
What are the benefits of an at home sleep test?
Doing a sleep apnea test at home has several advantages over a PSG in a sleep lab, such as:
Convenience: You can do the test in your own bed and avoid traveling to a clinic or hospital. You can also choose when to do the test according to your schedule and preference.
Comfort: You can sleep in your usual position and environment without wires or electrodes attached to your head and body. You may feel more relaxed and less anxious than in a lab setting.
Cost: An at home sleep test is typically cheaper than a PSG, which can cost thousands of dollars. Depending on your insurance coverage and provider, you may pay little or nothing out of pocket for an at home sleep test. However, it is unlikely that you will find an entirely free at home sleep apnea test.
Accessibility: An at home sleep test may be more available and accessible than a PSG, especially in rural or remote areas where sleep labs are scarce or have long waiting lists.
What are the disadvantages of an at home sleep test?
An at home sleep test also has some drawbacks and limitations compared to a PSG in a sleep lab, such as:
Accuracy: An at home sleep test may not be as accurate or reliable as a PSG, which measures more parameters and is supervised by trained technicians. An at home sleep test may miss some episodes of apnea or hypopnea, or overestimate or underestimate their severity. It may also fail to detect other types of sleep apnea such as central sleep apnea (CSA) or complex sleep apnea (CompSA), which involve problems with your brain's control of your breathing.
Quality: An at home sleep test may have lower quality or incomplete data due to technical issues, user errors, or poor signal. The device may malfunction, fall off, or run out of battery during the night. You may also move around, change positions, or remove the device unintentionally. This can affect the validity and interpretation of the results.
Feedback: An at home sleep test does not provide immediate feedback or support during the night. You may not know if the device is working properly or if you are using it correctly. You may also have questions or concerns that cannot be addressed until you receive your report.
Follow-up: An at home sleep test does not guarantee that you will receive appropriate treatment or follow-up care for your OSA. You may have to wait for a long time to get your results, see a doctor, or start therapy. You may also have difficulty finding a provider who accepts your results or offers the treatment options that you need.
Is it better to do a sleep study at home or in a lab?
Deciding between an at home sleep test and an in-lab sleep study depends on individual circumstances and preferences. At-home sleep tests (HSATs) offer convenience, affordability, and the comfort of sleeping in your own bed. They are suitable for individuals with a high likelihood of moderate to severe sleep apnea and no other significant health concerns.
In contrast, in-lab sleep studies provide comprehensive monitoring and are ideal for complex or potentially severe cases. They are supervised by trained technicians and offer more data, making them suitable for diagnosing various sleep disorders beyond sleep apnea. Ultimately, consulting with a healthcare provider is essential to determine the most appropriate option based on your specific symptoms, medical history, and insurance coverage.
How to prepare for an at home sleep test?
To ensure that your at home sleep test goes smoothly and produces accurate results, you should follow these tips:
Read and follow the instructions carefully. Make sure you understand how to set up, use, and return the device. If you have any questions or doubts, contact the provider before the test.
Avoid alcohol, caffeine, nicotine, and medications that can affect your sleep or breathing on the day of the test. These substances can interfere with the quality and accuracy of the data.
Maintain your normal routine and habits on the day of the test. Do not nap, exercise, eat, or drink too much or too little before the test. Go to bed and wake up at your usual times.
Choose a comfortable and quiet place to sleep. Make sure the room is dark, cool, and free of distractions such as noise, light, pets, or people. Avoid sleeping on a couch, recliner, or air mattress.
Attach the device correctly and securely. Follow the instructions on how to place and adjust the device on your body. Make sure it is not too loose or too tight. Check that it is working properly and has enough battery power.
Sleep as normally as possible. Try to relax and fall asleep naturally. Do not worry about the device or the results. Do not look at the device or check the time during the night.
How to interpret the results of an at home sleep test?
The results of your at home sleep test will be interpreted by a provider or a sleep physician who will send you a report with your diagnosis and recommendations. The report will include several metrics that indicate how well you breathe during sleep and how severe your OSA is. Here are some of the most common metrics:
Apnea-hypopnea index (AHI): This is the number of times per hour that you stop breathing (apnea) or have shallow breathing (hypopnea) for at least 10 seconds. A normal AHI is less than 5 events per hour. An AHI of 5 to 15 indicates mild OSA; 15 to 30 indicates moderate OSA; and more than 30 indicates severe OSA.
Oxygen desaturation index (ODI): This is the number of times per hour that your blood oxygen level drops by 4% or more from its baseline value. A normal ODI is less than 5 events per hour. A higher ODI indicates more frequent and severe drops in oxygen levels due to apnea or hypopnea.
Respiratory disturbance index (RDI): This is the number of times per hour that you have any type of breathing disruption during sleep, including apnea, hypopnea, snoring, arousals, or respiratory effort related arousals (RERAs). A normal RDI is less than 5 events per hour. A higher RDI indicates more frequent and subtle disturbances in your breathing that may affect your sleep quality.
Treatments for sleep apnea
If you're diagnosed with Obstructive Sleep Apnea (OSA) after a sleep test at home, there are several crucial steps to take for effective management.
First, discuss the results and treatment options with your healthcare provider. Depending on the severity of your OSA and individual circumstances, treatment may include lifestyle modifications, such as weight loss or positional therapy, or the use of a Continuous Positive Airway Pressure (CPAP) device to help keep your airway open during sleep.
It's essential to follow your healthcare provider's recommendations closely to improve your sleep quality, overall health, and quality of life. Regular follow-up appointments and ongoing monitoring may be necessary to ensure that your OSA is effectively managed and any necessary adjustments to your treatment plan are made.
Get tested for sleep apnea
Sleep apnea can be a serious and life-threatening condition if it continues to go undiagnosed. If you suspect you have sleep apnea, at-home sleep tests offer a convenient and effective way to diagnose the condition from the comfort of your own bed. By consulting with a healthcare provider, obtaining the necessary equipment, and following the instructions carefully, you can take a significant step toward better sleep and improved overall health.
FAQs
Q: Can I perform an at-home sleep test without a prescription?
No, at-home sleep tests require a prescription from a healthcare provider to ensure accurate diagnosis and appropriate follow-up care.
Q: How long does it take to get the results of an at-home sleep test?
Results typically take a few days to a couple of weeks to be reviewed by healthcare professionals.
Q: What should I do if my at-home sleep test indicates sleep apnea?
If you receive a positive diagnosis for sleep apnea, consult with your healthcare provider to discuss treatment options. Treatment may involve lifestyle changes, CPAP therapy, or surgery, depending on the severity of your condition.
Q: Are At-Home Sleep Tests Covered by Medical Insurance?
Yes, coverage for at-home sleep tests, also known as home sleep apnea tests (HSATs), varies depending on your insurance plan and the medical necessity. In many cases, insurance covers these tests, but you may need a prescription, and you might be responsible for deductibles or co-payments. It's crucial to check with your insurance provider, ensure your healthcare provider documents the medical necessity, and consider in-network providers for better coverage. If denied initially, you can appeal with additional medical documentation. Ultimately, understanding your insurance plan's specifics is key to maximizing your benefits for sleep apnea diagnosis.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaDirect sources and distributes a wide range of treatment solutions, including assistive CPAP equipment and sleep solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add CPAP supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 780-1508 between 8:00 am - 10:00 pm EST daily. Get in touch today.
LEGAL DISCLAIMER: Material in this newsletter is only 1) provided for general health education and informational purposes, and to provide references to other resources; it may not apply to you as an individual. While Apria believes that the information provided through this communication is accurate and reliable, Apria cannot and does not make any such guarantee. It is not intended to be a replacement for professional medical advice, evaluation, diagnosis, services or treatment (collectively, "medical treatment"). Please see your healthcare provider for medical treatment related to you and your specific health condition(s). Never disregard medical advice or delay seeking medical care because of something you have read on or accessed through this website. Reading this newsletter should not be construed to mean that you have a healthcare provider/patient relationship with Apria.
Related Content
Sleep Apnea and Pulmonary Hypertension
Sleep apnea stinks. For many reasons. You wake up in the middle of the night gasping for breath. You sound like a lumber yard of snores while you slee ...
Sleep Apnea and Sleep Cycles: How to Improve Your Quality of Sleep
If you suffer from sleep apnea, you may have trouble getting a good night's rest. Sleep apnea is a condition that causes your breathing to stop and st ...
How Sleep Apnea May Cause Headaches
Headaches are a bit like ice cream. They come in a lot of flavors, and you can pick them up in a variety of places. Ice cream may come from a grocery ...